Blepharitis (Child)
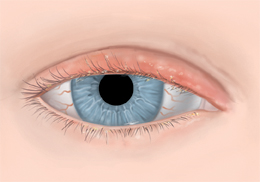
Blepharitis is inflammation of the eyelid. It results in swelling of the eyelid, and it's often caused by a bacterial infection or a skin condition. Blepharitis is common. There are two types:
In addition to swollen eyelids, symptoms of blepharitis can include thick, yellow, dandruff-like scales that stick to the eyelid. There may be oily patches on the eyelid. The eyelashes may be crusted (with dandruff-like scales) when your child wakes up from sleeping. The irritated area may itch. The eyelids may be red. The eyes can be red and burn or sting. The eyes may tear a lot, or they may be dry. Some children can become sensitive to light or have blurred vision. Symptoms of blepharitis can often cause a child to become irritable.
Infected eyelids are treated with good lid hygiene and careful removal of crusts. In severe cases, blepharitis may need to be treated with antibiotics. An episode may take 2 to 8 weeks to go away.
Causes
Other causes of blepharitis may include:
-
Problems with the oil glands in the eyelid (meibomian glands)
-
Dandruff of the scalp and eyebrows (seborrheic dermatitis)
-
Acne rosacea (a skin condition that causes redness of the face)
-
Eyelash mites (tiny organisms in the eyelash follicles)
-
Allergic reactions to cosmetics or medicines
Home care
Medicine: You may be given antibiotic eye drops or ointment, artificial tears, and/or steroid eye drops to treat your child’s infection. Follow all instructions for giving this medicine to your child. If your child has pain, you can give them pain medicine as advised by the health care provider. Don’t give your child aspirin. Aspirin can cause rare but very serious problems in children. Don’t give your child any medicine for this condition without first asking their provider.
-
Using eye drops. Apply drops in the corner of the eye where the eyelid meets the nose. The drops will pool in this area. When your child blinks or opens their eyelid, the drops will flow into the eye. Use the exact number of drops prescribed. Be careful not to touch the eye or eyelashes with the dropper.
-
Using ointment. If both drops and ointment are prescribed, give the drops first. Wait at least 3 minutes, then apply the ointment. Doing this will give each medicine time to work. To apply the ointment, start by gently pulling down the lower lid. Place a thin strip of ointment along the inside of the lid. Begin at the nose and move outward. Close the lid. Wipe away excess ointment from the nose area outward. Have your child keep the eye closed for 1 or 2 minutes so the ointment has time to coat the eye. Eye ointment may cause temporary blurry vision. This is normal. Apply ointment right before your child goes to sleep. In infants, the ointment may be easier to apply while your child is sleeping.
General care
-
Wash your hands carefully with soap and clean, running water for at least 20 seconds before and after caring for your child’s eyes. If you need a timer, sing the "Happy Birthday" song twice.
-
Apply a warm compress or a warm moist washcloth to your child's eyelids for at least 1 minute, 2 to 4 times a day. Then wipe away scales or crust from the eyelids.
-
After applying the warm compress, gently scrub the base of your child's eyelashes for almost 15 seconds per eyelid. Do this with your child’s eyes closed, using a moist eyelid cleansing wipe, clean washcloth, or cotton swab. Ask your child's health care provider about products (such as nonirritating baby shampoo) to help clean the eyelids.
-
You may be instructed to gently massage your child's eyelids to help unblock eyelid glands. Follow all instructions given by the provider.
-
Clean the eyelid if it has a lot of crusts. Use warm water and a small amount of mild baby shampoo (about 1/2 teaspoon to 1 cup of warm water) or an eyelid scrub recommended by your child’s provider. Put the solution on a clean washcloth or gauze pad. Gently clean the lashes and lid edges. Don’t touch the eye. Be gentle to avoid causing irritation. Carefully rinse if shampoo is used.
-
Try to prevent your child from rubbing their eyes.
-
Unless told otherwise, regularly clean your child's eyelids (while they are closed) as directed by the provider. Blepharitis can be an ongoing problem.
-
Your child should not wear eye makeup until the inflammation goes away, or as directed by your provider. When cleared to wear makeup, the old makeup should be thrown away and new makeup purchased.
-
Your child shouldn't wear contact lenses until they complete treatment.
-
Encourage your child to wash their hands regularly. This helps to reduce the chance of dirt and bacteria coming in contact with the eyelid. Teach your child when and how to correctly wash their hands.
Follow-up care
Follow up with your child’s health care provider, or as advised. Blepharitis requires regular follow-up care. Your child may be referred to an eye care provider who specializes in treating eyes (an optometrist or ophthalmologist) for further evaluation and treatment.
When to get medical advice
If your child is usually healthy, contact their health care provider right away if:
-
Your child has a fever (see “Fever and children" below).
-
Symptoms get worse.
-
Your child has eye pain.
-
Redness increases in the white part of the eye.
-
Your child has a change in vision (trouble seeing or blurring).
-
The eyelids start draining pus or blood.
-
Eyelid swelling, redness, irritation, or pain gets worse.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years old, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The health care provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Contact the health care provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older